We’ve learned enough in the last two years to revisit the supplementation advice from our book, and toward that end I am starting a series on micronutrients.
I’ve recently been looking at some papers studying the effects of food fortification with micronutrients. These changes provide a sort of “natural experiment” which may provide insight into the benefits and risks of supplementation.
Fortification of Food
Grain products are the most important category of fortified foods. Industrially produced baked goods must generally use enriched flour, and Wikipedia (“Enriched Flour”) tells us what they’re enriched with:
According to the FDA, a pound of enriched flour must have the following quantities of nutrients to qualify: 2.9 milligrams of thiamin, 1.8 milligrams of riboflavin, 24 milligrams of niacin, 0.7 milligrams of folic acid, and 20 milligrams of iron.
This is an ironic choice of nutrients. While thiamin and riboflavin are harmless, niacin, folic acid, and iron are three micronutrients we recommend NOT supplementing in the book. Another nutrient we recommend NOT supplementing, vitamin A, is also a fortified nutrient, although not in flour.
Perhaps not even for that!
A history of nutrient fortification over time can be found at this USDA site. Enrichment has a long history, but the amount of fortification has increased substantially since the 1960s. Enrichment mixtures were added to rice, cornmeal/grits, and margarine beginning in 1969, and to ready-to-eat cereals, flour, and semolina beginning in 1973. Inclusion of high levels of folic acid in all enriched foods became mandatory in 1998.
You may have noticed that when putting raw rice in water, a white powder comes off the rice. This is the enrichment mixture which contains folic acid. According to the American Rice Company (hat tip: Matthew Dalby),
The enrichment mixture is applied to rice as a coating. Therefore, it is recommended that rice not be rinsed before or after cooking and not be cooked in excessive amounts of water and then drained. The enrichment … would be lost.
This is useful information: We can remove the enrichment coating by rinsing rice before cooking. That may turn out to be a good idea!
The Contribution of Fortification to Nutrient Intake
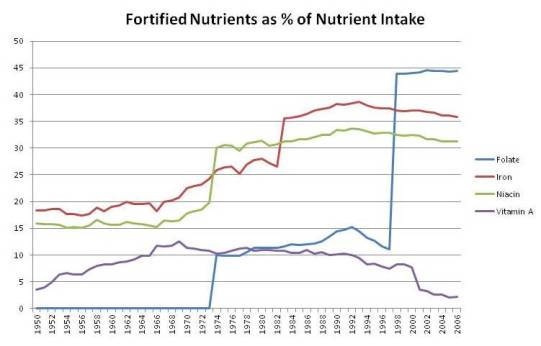
Using USDA data for the four nutrients most likely to be harmful in excess, I made up a chart of the contribution of fortified nutrients to total nutrient intake among Americans. It looks like this:
You can see sharp rises in fortified niacin and folic acid in 1973, in iron in 1983, and again in folic acid in 1998. By 1998, folic acid in fortified foods constituted 44% of all dietary folate, and enrichment mixtures provided one-third of all iron and niacin. Fortified vitamin A provided about 10% of all dietary vitamin A from 1964 through 2000.
Folic Acid
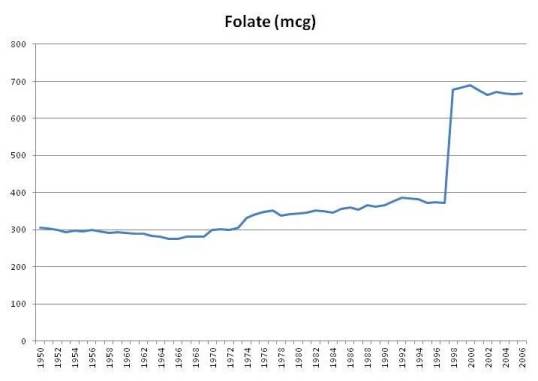
Here is a chart of per capita daily intake of fortified folic acid plus natural food folate in the United States since 1950:
Folate intake from foods has always been around 300 mcg per day, and jumped sharply when folic acid intake became mandatory in 1998. The USDA estimates that intake of folate, including folic acid, jumped from 372 mcg per person per day in 1997 to 678 mcg in 1998, and has remained above 665 mcg ever since (source).
For those who eat a lot of wheat products, intake may be even higher. A pound of enriched white flour has 770 mcg folic acid along with its 1660 calories. If Americans were getting 372 mcg folate from food prior to folic acid fortification, then someone eating a pound of enriched wheat products per day would be getting about 1,142 mcg folate from all food sources.
It’s not uncommon to eat substantial amounts of enriched wheat. The typical American eats 474 g (1800 calories) carbohydrate per day. Most of that is from enriched grains. Those eating industrially produced breads, cookies, crackers, and breakfast cereals may have a very high folic acid intake.
Add in a multivitamin – most multivitamins have 400 mcg and prenatal vitamins have 800 mcg – and a sizable fraction of the population has a folate intake of 1,500 to 1,900 mcg per day, 1200 to 1600 of it as synthetic folic acid. This is well above the tolerable upper limit (UL) for folic acid of 1000 mcg (Wikipedia, “Folate”).
Averaged over all Americans, folic acid from fortified foods comprises 44% of all food-sourced folate, but for Americans taking a multivitamin folic acid becomes 65% of all folate and, for those taking a prenatal vitamin, 75%.
There are several potential health problems that could arise from excessive intake of folic acid, and I’ll explore a few in this series.
Iron and Niacin
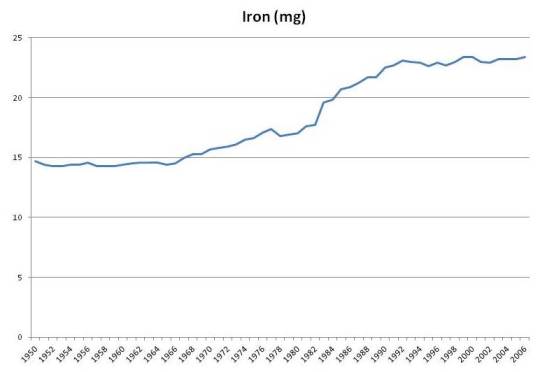
Iron intake has risen by about 50% due to fortification:
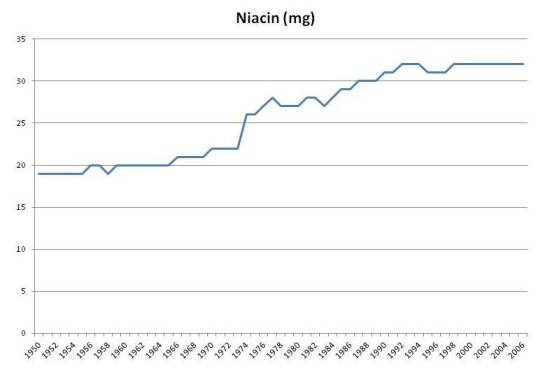
Niacin intake has also risen about 50%:
These two nutrients have similar concerns:
- An excess of each promotes infections. Niacin (in the NAD+ form) is the rate-limiting factor in bacterial metabolism. Iron is a critical mineral for oxygen handling and is needed by most infectious pathogens; in fact the immune response tries to lock up iron in ferritin during infections.
- Both niacin and iron are involved in oxygen handling during metabolism and an excess of each can aggravate oxidative stress.
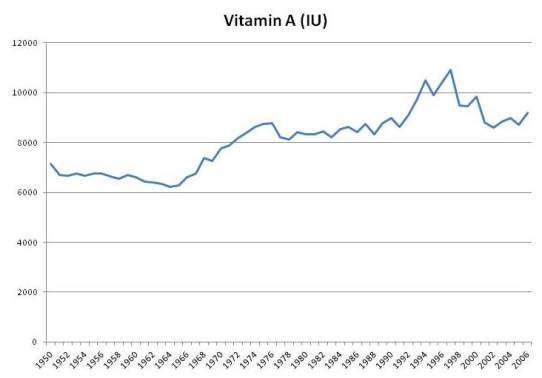
Vitamin A
Although fortification never increased vitamin A intake by more than 10%, it may serve as a marker for consumption of artificial sources of vitamin A from supplements. Moreover, total food intake of vitamin A was apparently affected by fortification; food intake of vitamin A rises in the 1960s when fortification was growing, and falls after 2000 when intake of fortified vitamin A decreased:
In the book we noted studies showing that people whose intake of vitamin A was above 10,000 IU/day tended to have higher mortality. This was most commonly observed in people taking multivitamins.
There was a period of enthusiasm for vitamin A supplementation between the 1960s and 2000. Multivitamins had more vitamin A in that period. After studies showed negative results, the vitamin A content of multivitamins was reduced.
It is possible that the source of problems may not be vitamin A per se, but degradation products of vitamin A. I’ve previously blogged about how vitamin A plus DHA (a fatty acid in fish oil) plus oxidative stress can produce highly toxic degradation products (see DHA and Angiogenesis: The Bottom Line, May 4, 2011; Omega-3s, Angiogenesis and Cancer: Part II, Apr 29, 2011; Omega-3 Fats, Angiogenesis, and Cancer: Part I, Apr 26, 2011).
Naturally occurring vitamin A in foods is located in lipid fractions and protected from oxidation by accompanying antioxidants (eg vitamin E) and oxidation-resistant lipids. Vitamin A from fortification is not so carefully protected. The Food and Agriculture Organization of the United Nations comments:
Foods which have been successfully fortified with vitamin A include margarine, fats and oils, milk, sugar, cereals, and instant noodles with spice mix. Moisture contents in excess of about 7-8% in a food are known to adversely affect the stability of vitamin A. Beyond the critical moisture content there is a rapid increase in water activity which permits various deteriorative reactions to occur. Repeated heating, as may be experienced with vegetable oils used for frying, is known to significantly degrade vitamin A. The hygroscopic nature of salt has prevented its use as a vehicle for vitamin A fortification in countries of high humidity. In trying overcome this problem, a new vitamin A fortificant, encapsulated to provide an additional moisture barrier, was evaluated with limited success. The cost of using highly protected fortificants can be prohibitive in many cases.
There aren’t many foods that don’t contain 7% water, or acquire it after fortification, so degradation is a real concern.
Vitamin A in multivitamins may also be exposed to degradation. The possibility of vitamin A degradation, especially in combination with DHA from fish oil and oxidative stress, is why I’m skeptical of the health merits of fermented cod liver oil.
Conclusion
I think exploring the effects of fortification will be an interesting topic.
We will consider whether fortification may play a role in various diseases that have become more common since 1970 or 1998, such as obesity, diabetes, and autism.
And we will consider what the health effects of food fortification may tell us about how to optimize micronutrient supplementation.












But why supplement iron in wheat in the first place (for instance)?
My understanding is that it was to combat anemia… Isn’t pernicious anemia one of the typical symptoms of celiac?
Might cutting wheat out of the diet reduce or alter the need for iron? (One would imagine swapping wheat for meat would certainly reduce the need to supplement iron…)
Paul, can you expand on this statement at all? ” is why I’m skeptical of the health merits of fermented cod liver oil.” I have started taking it, I do keep it refrigerated to try to minimize degradation but will that be enough?
Thanks,
Justin
Hi Tuck,
As far as I can tell, the rationale of the fortifiers was to make white flour have the same iron content as whole wheat, even if the whole wheat iron is locked away in phytate.
Interesting thought about cutting wheat reducing the need for iron.
Hi Justin,
Well, the fermentation process itself exposes the cod liver oil to bacterial enzymes and compounds that can potentially lead to degradation of food components. After all, the bacteria have to degrade the cod liver oil to feed on it. In generally I think fermented animal foods are much riskier than fermented plant foods. The one exception is dairy which contains sugars specifically designed by evolution to feed probiotic flora.
I don’t have any data on this, it’s just a suspicion. But I have heard a few anecdotal reports of people having trouble on fermented cod liver oil.
Best, Paul
I look forward to your series on fortification and supplementation, and especially your new recommendations. I was in the midst of evaluating multivitamins, and will put getting a new one on hold.
I have been itchy about enriched foods for awhile now. I am particularly leery of iron. What do you think of the iron gout relationship? I know that there have been some studies showing that people who go from traditional diets high in fruit to western style diet full of flours and drinkable fructose have been shown to have lots of problems with gout. Do you think that fortification may play a role in these western conditions?
Hi Jeremy,
I’m getting tempted to give up multivitamins entirely and just do individual supplements, or perhaps a multimineral plus individual supplements. I’ve never found a multi I could fully believe in.
Also, our food keeps getting more nutrient rich, and I’m thinking we can reduce the frequency of supplementation, maybe to once a week for most nutrients.
Hi Meredith,
I haven’t looked into gout, it’s a great question. I’ll keep it in mind and look for papers.
Regarding your concerns over niacin, could you provide some citations? Do you have the same concerns with niacinamide? Thanks.
Hi David,
I’ll have a little to say about niacin later. Yes, I have the same concerns with niacinamide. Niacinamide is at least free of the liver toxicity that niacin has, but that matters at higher doses.
Hi Paul:
As you know folic/folate was put in pre-natal vitamins to protect against neural tube defects. With the enrichment of it found in flour, there must have been some reason for the high levels of it in multis for pregnancy. Pregnant women’s eating habits can be erratic, so maybe that is why there is so much of folic in the multi’s
If one is following a PHD then they are not getting any of the enrichment/fortification because with the exception of rice followers are not ingesting high levels of the vitamins you have discussed.
My understanding of the growth in multi supplementation has been in large part a response to fruits and veggies being bought at the grocer, sitting on the shelf and not containing the amount of vitamins as freshly picked from the garden/tree would have.
I think you are correct about going in the direction of mineral supplementation with select vitamin supplementation. Be interested in your fully developed thoughts on that. I think D,K, a B complex with no more than 400mcg of folic acid might make sense. I’m not sure how much of the “B’s” you can from PHD if you eat no grain except rice, and if you eat limited rice, but mostly potatoes is that sufficient for your “B” needs? Also, if someone takes a multi, what do you think the maximum amount of A should be along with beta-carotene levels?
Excellent review!
Hi steve,
I think we’re going to track our food for a week and see how much we’re getting of various nutrients. I haven’t really figured out what the new advice will be yet. There might be a few adjustments to our plateau ranges, and then we’ll measure what a PHD-according-to-the-food-plate diet provides, and think about the best way to get everything in range.
Re folate, I don’t think you need a lot of folate to prevent neural tube defects. Any real-foods Paleo-type diet (as opposed to a soda and bread diet) should do it.
As therapeutic use of niacin involves amounts of 1,000mg/day or more long-term, I don’t believe that 32mg/day would/could be harmful.
@Nigel, the RDA fwiw is half that.
Hi Paul –
What’s your opinion on active folate (l-methylfolate). If you look at the chemical pathway toward glutathione production methylation is a major limiting step (both on folate and B12). (i’m not an expert) Something like 40% of Caucasians have defect in this gene that makes them deficient in activating folate and b12 – i’m curious if active folate contributes to cancer like you say folate does. If you search the net a bit you’ll also find a lot of sites that speak about women having a lot of miscarriages might be due to their MTHFR mutation and slow methylation. People with this gene mutation get high homocystine and it contributes to all sorts of health problems. Incidental note, I’m currently living in Austria and they fortify with active folate instead of regular folate. http://mthfr.net/
-Steve
Hi Nigel,
That’s part of what makes it interesting.
Hi Stephen,
Genes don’t reach 40% of a population unless they have benefits as well as costs, and supplementation didn’t start recently so I don’t think the benefit of the gene is to compensate for supplemental folic acid. So I’m skeptical that that gene variant is unhealthy on a healthy diet.
I’ll be discussing this, but I think the miscarriages result from low choline intake rather than low folate.
Hi Paul-
I found a multi,”Oxylent” that seems relatively harmless,and has a nice mineral profile.Perhaps that would be a good basis with a few individual supplements.I have emailed them with a few questions and they are very open to continued discussion…might be worth a look.
Hi Paul – I don’t think my comment on active folate came across completely. When a person takes in folate it has to be activated by methylation so that cells can use the folate further in their metabolic processess. People with mutations on the MTHFR gene are slow at activating folate – I think I read that the dietary non-activated folate can build up in the persons system and I’m curious if this is what contributes to the increased cancer. Other things that are related to this MTHFR defect are poor detoxification, especially of heavy metals, and poor immune function. This in turn often contributes to gut biofilms that are populated with pathogenic yeasts, bacteria and parasites. 98% of people diagnosed with Autism have at least one of the common defects on this gene. People with Aspergers tend to have it…its a long list of ‘traits’ that is related to the MTHFR gene defect and you write about a lot of them (including autism and the biofilm problems). Thought you’d be interested. There’s a ton of papers published its a pretty hot topic right now.
-Steve
Hi Stephen,
Yes, you are making a great point. Folic acid/folate needs to be methylated, so you need methyl donors, eg choline. If people have a low choline:folate ratio they will get into trouble.
This is great background for what I’ll be writing about soon. Thanks for the tips.
So just to get things straight, you are suspicious of fermenting cod liver oil because it could lead to the degradation of vitamin A, I get that, so what about molecular distillation? And what if it is a combined with enough vitamin E to prevent oxidation?
I know that cod liver oil would be better than isolated Vitamin A, but could it still pose a problem? I would only be consuming the RDA of Vitamin A from it.
Hi Paul,
Something I’ve been wondering about for a while now is having surety on exactly what is getting absorbed from the gi and intestinal tract on a per person basis, i.e. one guy due to gut problems/degradation absorbs only 1/2 of a particular nutrient compared to the next guy for the ingestion of the same quantity. Also, food interactions and competition limiting global intake zinc/copper as an example and throwing of recommendations for intake.
Hi Stabby,
I’d be willing to consume fresh cod liver oil as an alternative source of vitamin A and omega-3 fats.
Hi Perry,
It’s a good question. It would be nice if we had good measurement methods for mineral/nutrient status and could monitor them. I know you can get hair mineral analysis and the like, but I have no experience with it.
It is hard to recommend specific micronutrient intakes for the reasons you mention, different people will find different amounts optimal.
I hope this has not been mentioned already, but there is a very interesting paper on the possible role of b-vitamin fortification in the obesity epidemic
Hi Adel,
Yes, that’s one I intend to discuss. It won’t convince Nigel but it is entertaining.
right, the argumentation is everything else than conclusive, but this is still an interesting hypothesis and one where we actually don’t have much “real” (=non epidemiological) data… obviously the “enriched” foods are in and out of themselves a potential problem, so that from studies like this you cannot comment on the effects of “high” dose b-vitamins
specifically with reference to niacin, though, I see more and more evidence that everything that many of the “medicinal” or supplemental approaches to lower cholesterol (like niacin) have profound negative effects on insulin sensitivity
interestingly this effect appears to be of transient nature, cf.
Thanks, Dr Andro. I’ve seen niacin induction of insulin resistance in various places but haven’t looked into it its significance yet. Previously, in talking about how to raise HDL, I’ve recommended using coconut oil induced ketosis rather than niacin – niacin raises HDL by acting on a ketone receptor, and ketones are a much safer way to go.
I have definitely noticed that when I add rice to water, the water becomes a murky white. However, I now purchase only unfortified rice and the when I add the rice to water a white powder still comes off. This leads me to believe that I’m just removing starch. I do think washing fortified rice removes some of the enrichment coating, but I don’t think the murkiness alone denotes anything about that.
Yay, I loves me cod liver oil. And vitamin E.
This all reminds me that there is a new review of controlled trials for antioxidant-type supplement that claims that none of them are any good. I remember your commentary on observational studies and it was great, but these are placebo-controlled trials http://www.sciencedaily.com/releases/2012/03/120322174621.htm?utm_medium=twitter&utm_source=twitterfeed
I suppose it would depend on the form of the nutrient and there is little effort to distinguish between them. Vitamin A supplements may get degraded as you mentioned, but that may not be a criticism of cod liver oil, and there are many types of vitamin E, synthetic forms are invariably treated as synonymous with natural forms and the different types are all called “vitamin e” too. Byron Richards says that synthetic beta carotene is different from the kind he uses. Richards rants about this here http://www.wellnessresources.com/health/articles/natural_vitamin_e_dramatically_reduces_heart_disease/
Interestingly when looking at all of the data from the study he cites there appears to be evidence of a synergy between vitamin c and e, which seems pretty obvious. When vitamin c and e are combined instance of stroke goes down quite a bit, when vitamin e and c have little impact by themselves.
Also I wonder if taking alpha-tocopherol even in its natural form could be detrimental because it’s not the form we’re used to getting.
As I remember, some types of selenium may not be good but others are, from the Chris Kresser article. Vitamin C is a tough one but many vitamin C supplements don’t even really contain vitamin c anymore http://www.foodproductdesign.com/news/2011/09/anti-caking-agents-don-t-protect-vitamin-c.aspx
I’m just sharing my thoughts because of the new review. And because PHD recommends vitamin c and selenium supplementation in some cases, which seems to be justified by some studies but not others. Of course that doesn’t mean that we should just consider it ambiguous and therefore all of them are useless all of the time so there, like some people are doing. Maybe it’s time for a sister series to this one to explore the supplement issue?
heh the life of a blogger, I know how it is, though. I don’t actually expect a series on this stuff in the near future, it’s just a possibility. Although there is no shortage of topics to write about.
Hi Stabby,
The Science Daily story you link is about plant antioxidants (resveratrol, genistein) in vitro. So far as I know, it doesn’t show anything negative about human antioxidants (eg zinc, copper, vitamin C).
I think you’re referring to the recent Cochrane Review (http://www.ncbi.nlm.nih.gov/pubmed/22419320). I haven’t read it yet, but the abstract mentions only vitamins A and E as showing significant harm. Those are compounds where the supplemental forms may be quite different than the natural food forms.
Selenium is tricky because it’s so dangerous if you get too much, and food amounts are highly variable.
I am planning to survey the supplement issue fairly thoroughly, but not sure how soon it will get up on the blog.
Best, Paul
As you write more about micronutrient supplements, Paul, it would be great if you could talk a little about the many additives in supplements (e.g. stearic acid, stearates, and the like, calcium phosphate, silicon dioxide, coatings and glazes…), and identify the ones you consider potentially problematic.
I am concerned that we may let down our guard too much when we take supplements, ingesting industrial gunk that we would never tolerate in food.
Heh, yes I meant that review. Could have sworn that link was going to be the one!
Sounds great, I look forward to it.
Stephen’s question on active folate is a good one. My 10 yo daughter is being treated for a lyme/bartonella infection and her LLMD is supplementing her with the B6 metabolite P-5-P, L-methylFolate and methylB12 to address the MTHFR defect that is so prominent in a lot of kids with lyme induced autism and immune disregulation. We haven’t run the test yet, but this is intriguing to me. My daughter is responding well to treatment; her speech, executive function, handwriting, sound/light sensitivities have improved greatly with antibiotics and supplementation, and the ~80% implementation of your diet. I have been questioning our multivitamin supplementation lately as it lacks the methylated forms, even though we try to eat lots of egg yolks. I am looking forward to you addressing this question. Thank you so much for your hard work, you are helping so many.
Thank you, Louise, I’m glad your daughter is doing well.
I also take methylb12 (with nac) for bad fibro. Just started so not sure if it helps
An article in Life Extension Foundation magazine March 2012 issue is titled “EXCESS IRON and BRAIN DEGENERATION: The Little-Known Link” (link here):
http://www.lef.org/magazine/mag2012/mar2012_Excess-Iron-Brain-Degeneration_01.htm
Article seems related to the risky iron fortification of food experiment.
Hmm… whenever I read the words “vitamin A” this reminds me that there is a crucial and in my eyes detrimental misunderstanding which equates “beta carotene” to “vitamin A”; now let’s see how that fits the current context:
everybody is popping (mostly useless / if not detrimental) multivitamins these days with whopping doses of beta carotene in it,
a) following the mainstream misconception that you cannot overdose on “water soluble” vitamins,
b) assuming that your body will make just enough of “real” vitamin A (=retinol) from it, as it needs, and
c) ignoring that “not all vitamin(s) A (and also C)” are made equal (cf. previous blogpost of mine @ http://suppversity.blogspot.de/2011/10/are-there-pro-oxidant-cytotoxic-and-dna.html)
specifically wrt to b) the following recently published study is of particular interest to me
Now, while we have a decrease in adiposity, here, it is somewhat unsettling that supplemental beta carotene increased the incidence of “real” vitamin A deficiency.
I wonder what would happen if you add the currently hailed “minimal” dose of 2,000IU vitamin D per day on top of the beta-carotene overload from supplements and fortified foods
Paul,
One distinctive piece of advice you give is to supplement copper. Are you familiar with the survey articles of Brewer on the potential toxicity of copper (and iron)?
http://www.ncbi.nlm.nih.gov/pubmed/17259340
http://www.ncbi.nlm.nih.gov/pubmed/19968254
Jeremy
I was rooting around pubmed earlier and I found this study on vitamin c (still on the subject of antioxidants) http://www.ncbi.nlm.nih.gov/pubmed/10527771 It looks like 1g isn’t sufficient to prevent some of the negative effects from smoking (don’t worry I’m not planning on doing a “mitigating the deleterious effects of chain-smoking” series…, heh) but 2g has some efficacy, suggesting some sort of saturation point where levels are too high to be cleared. Of course this all begs the question of whether or not it’s healthy to do that, especially long-term, this is only an cute study, but the point may be that if people wish to reap the benefits of vitamin c supplementation maybe the best effects come after a certain dosage. I’m not sure if anyone has ever consumed a natural diet with that much, but maybe there’s a difference between natural and supplemental.
Just some thoughts. In that study that you cited in the book where vitamin c extended lifespan by 7 years what dose did they take? And what might the deal be when that one was positive but others are negative? Besides the possibility of poor supplement quality and degradation of the vitamin c.
@Jeremy: I see your point, but as so often the dosage makes the toxin. And within the health and fitness community where people are taking their high potency multi with 15mg of zinc and their ZMA pre-bed with another 30-50mg (depending on brand) it is unfortunately more likely that they get zinc-toxic and have low iron and low copper, than vice versa
@Louise: its nice to hear from another MTHFR patient on this site. I am ‘clinically measured’ to be on the Aspserger’s spectrum and a holistic doc in WA attributed it to me being compound heterozygous in C677T and A1298C (he said I had it ‘bad’ regarding my rate in activating b-vitamins in the glutathione production pathway). After suffering from gut disorders and social behavior problrms all my life the doc treated me with a biofilm protocol that is similar to a gut cleansing program that Paul has written about on this site. It included enzynattokinase as nattokinase, meetal chelators and antimicrobials. I saw slime, fungus balls, and worms leaving my body over the course of a month. the bad biofilm was gone. Next the doc started me on active forms of dilate and b-12…along with methyl donors like betaine and Dmg and choline. Also supplement with support nutrients on the glutathione pathway including p5p, sam-e, and nac. The docs argument is that I can take all the methyl donors in the world but if my genes are rate deficient in taking the methyl groups and activating my dietary folate and b12 then Ill have issues. hence the fact that we ‘short circuit’s the glutathione methylation issue by taking active folate and methyllb12 because its more appropriate for my individual biochemistry. Let me tell you-all my social awkwardness and gut problems have disappeared. after 20 years with this supplementation regimen. I really hope Paul will look into the MTHFR gene defects and rectify it against his diet better.
Hi Paul
Well done for all your work. I have recommended your site and book here,
http://her2support.org/vbulletin/showthread.php?t=24410&page=19 [PAJ: Specifically, http://her2support.org/vbulletin/showpost.php?p=267503&postcount=374%5D
but do have reservations on your views, as I understand your blog, on the pragmatic risk reward of moderate fish oil use in those that otherwise would manifest severe Omega 3:6 cellular membrane imbalances.
I agree whole food is the optimum option, however in our modern world, on a pragmatic risk benefit analysis I believe fish oil has health benefits for most on western diets. Most on western diets do not restrict their Omega 6 LA intake to maybe 2% of calories (pregnant women and those with serious infections illnesses may need more)but ingest maybe 8-10% of calories as Omega 6 LA.
Most people have an Omega 6 intake that far exceeds their Omega 3 intake, which is reflected in the Omega 3:6 composition of their cell membranes. Fats in the cell membranes are released in response to stress, immune function, tissue repair, reproduction etc and oxidized often by enzymes to bioactive products. These bioactive products have a range of roles. In very general terms the Omega 6s are connected with inflammation, and Omega 3s often moderate inflammation.
Excess inflammation is one of the root causes on western disease.
Taking fish oil helps address this imbalance, and so helps reduce inflammatory pressures.
Stored Omega 6 in fat tissue has increased from maybe 4% in the 1950s to maybe 10% plus and up to 25% in some modern populations. It takes several years to re-balance the profile of body fats, and during this time those with high Omega 6 stores will be releasing Omega 6 fats and so have a higher ratio of Omega 6 to 3, even if they have meantime significantly reduced their Omega 6 intake.
In people with massive Omega 3:6 imbalances I an open to the idea there maybe an argument to a short term kickstart in the form of a modestly higher intake of fish oil / oil fish and some plant based Omega 3 in the form of flax oil.
Not everybody eats fish, or has access to high quality natural oily fish, due to cost, availability etc. and then there are the wider issues as to global fish stocks, and pollution with heavy metals etc.
Most quality refined oils are free of such pollutants, but of course also lack the other important synergistic beneficial nutrients in fish.
Fermented fish oil was being used with health benefits long before the recent sharp rise in the prevalence of western inflammatory conditions.
I accept as you propose the ideal is eat adequate fish proportionate to your Omega 6 intake, moderate your Omega 6 intake, and in those circumstances, assuming no historic imbalances,or genetic predispositions, fish oil may indeed be no benefit and indeed could increase the risks of oxidative stress.
However as usual things are more complex, and some groups are genetically up to 40% less efficient in converting the plant based Omega 3s to the longer chain fats and particularly EPA and DHA, and so are more reliant on them. There is growing evidence that ‘Celts’ / shoreline peoples may be at higher but by no means exclusive risks of poor conversion, from which one could construct an argument that those people optimally need more long chain Omega 3 than the average.
I am not suggesting that the use of any refined food is without risks. However I suggest for those with historic Omega 6 imbalances, including significant amounts in stored fats, who do not for whatever reason have access to or wish to eat fish,(pollution risks – cost – availability) that moderate supplementation with fish oil (providing 1-2 grams EPA and DHA – not mega amounts) will help address the Omega 3:6 imbalance in the cell membranes, and so help address a basket of inflammatory issues.
Yes there may well be issues with fish oil when compared to the ingestion of Omega 3s from quality unpolluted fish, but I believe they are far outweighed by the benefits of fish oil consumption in those who would otherwise have severe Omega 3:6 imbalances.
I also believe that on the balance of probabilities addressing the Omega 3:6 imbalance for a vast array of reasons reduces the risk of inflammatory related ‘western’ conditions which includes a rising risk of many cancers. The Omega 3:6 imbalance is best addressed through whole foods, but pragmatically on a risk benefit basis in our complex resource pressured often increasingly polluted world I suggest for those who do not chose to reduce their Omega 6 intake, and or have access to fish / choose not to eat, fish oils have a place in improving health.
Hi Robert,
Thanks for your kind post, and your thoughts on the fish oil supplements. I’d like to see the fermented cod liver oil studied a bit in the literature before I would feel comfortable endorsing it.
Hi Paul,
Do you never recommend Iron even for menstruating women? I take 25mg 3X a week. Perhaps, I should stop? Thanks!
Hi Prof Dr Andro, Olaf, Jeremy, and Stabby,
Thanks for those links. Great reading material! I have my homework cut out for me.
Hi Helena,
Yes, I do recommend iron for menstruating and pregnant women. The level you’re taking is great.
Hello Paul-
I’m a little confused: Your diet plan says not to eat wheat, but is whole wheat unhealthy? My family eats whole wheat that we grind in our VitaMix from wheat berries. Is this not good for one’s body? You may have adressed this before, but this is my first time seeing your website.
Hi Shannon,
Yes, whole wheat may be worse than refined wheat, because the bran has about 50% more toxic proteins per unit weight than the kernel.
I would just avoid wheat entirely and stick to rice, potatoes, and other “safe starches.”
Hi Paul,
I haven’t used a multi in over 10 yrs; different times of day for different supps (calcium in afternoon, magnesium at night, etc.), and even different amounts on different days.
Whenever vit E occurs in food, it’s always all 4 tocopherols, leading me to conclude that they are the essential components (not different “forms”) of vit E. My E supp is liquid mixed tocopherols in a gelcap.
I’ve also concluded certain ratios matter a lot, which have been widely unrecognized (and therefore widely violated):
> You need at least as much calcium as magnesium, but not more than twice as much.
If 400 mg mag, then 400 – 800 mg cal; if 1000 mg cal (the RDA), then 500 – 1000 mg mag (I do NOT recommend one g mag!).
> You need at least as much omega-6 as omega-3, but not more than twice as much.
If 1000 mg o-3, 1000 – 2000 mg o-6; if 2000 mg o-3, 2000 – 4000 mg o-6.
> You need at least as much vitamin A as vitamin D, but not more than twice as much.
If 5000 IU vit A (the RDA), then 2500 – 5000 iu vit D; if 5000 iu D, then 5000 – 10,000 iu A.
@Shannon & Paul: I don’t know if anyone of you has ever thought about that (or Paul written about it), but did it ever occur to you that there is no whole grain in whole grain foods?
What I am hinting at here is that eating REAL whole grains and not products that are made of flour that was made from whole grains and 100x processed, would be “soaked” and “fermented” in your digestive tract before they were taken up; or they would pass through totally undigested. The processing process on the other hand, creates all sorts of micromolecules that would NOT occur when you chew the “whole grains” or when they are broken down enzymatically or “eaten” by bacteria.
@Jeffrey: You should no underestimate the amount of calcium you get from hard water (I calculated my intake from water to be ~600mg+, alone!) and greens – supplemental calcium is usually simply unnecessary. On the other hand, MG is currently among the most overhyped supps. It is as you see not a good idea to take more than 400mg – especially if you are on a paleo diet which often is pretty low in salt / hypotension and brain fog are usually the consequence of this practice.
I am with you on the vitamin E issue, though, if you are interested I have a collection of posts on E at the SuppVersity > http://suppversity.blogspot.de/search/label/vitamin%20E and also agree on the notion that ratios are more important in these days of overabundance than total intakes. That this is also true for B-vitamins is unfortunately 100% underappreciated by most people (too much B6, for example increases B5 excretion, etc.)
Hi Jeremy, Dr. Andro,
Great points. We’re eating bone broth a lot these days, that should supply plenty of calcium.
Dr Andro, I hadn’t considered that, but it seems quite likely. The grains evolved to evade digestion, and are small and numerous and hard for that purpose. The greater the integrity of the grain, the more likely they are to survive digestion intact.